When it comes to radiopaque lesions of the mandible, a thorough understanding is paramount. This article delves into the depths of this topic, providing a comprehensive overview that unravels the complexities of these lesions, their causes, diagnosis, and treatment options.
Get ready to embark on an enlightening journey into the realm of radiopaque lesions of the mandible!
Radiopaque lesions of the mandible, characterized by their ability to obstruct the passage of X-rays, are a diverse group of lesions that can arise from various etiologies. Understanding their nature and implications is crucial for accurate diagnosis and effective management.
Define Radiopaque Lesions of the Mandible
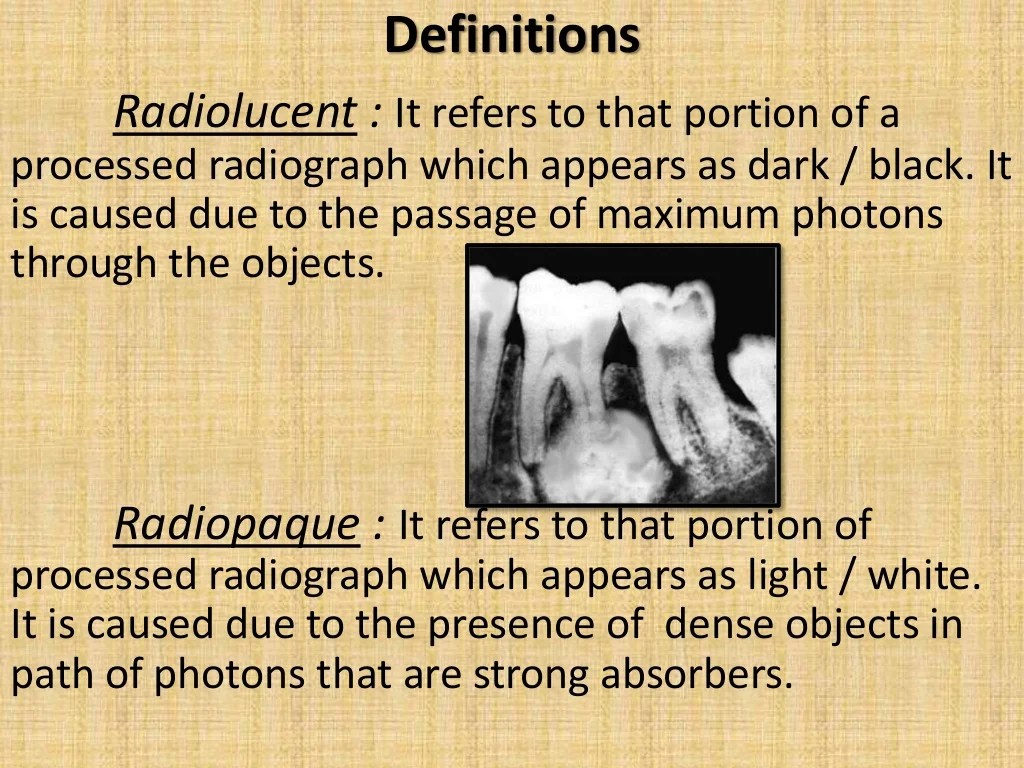
Radiopaque lesions of the mandible are areas within the jawbone that appear white or opaque on dental X-rays. These lesions indicate the presence of dense or calcified materials within the bone.
The mandible, also known as the lower jaw, is the bone that forms the lower part of the face. It consists of a horizontal body and two vertical rami that connect to the temporal bones of the skull.
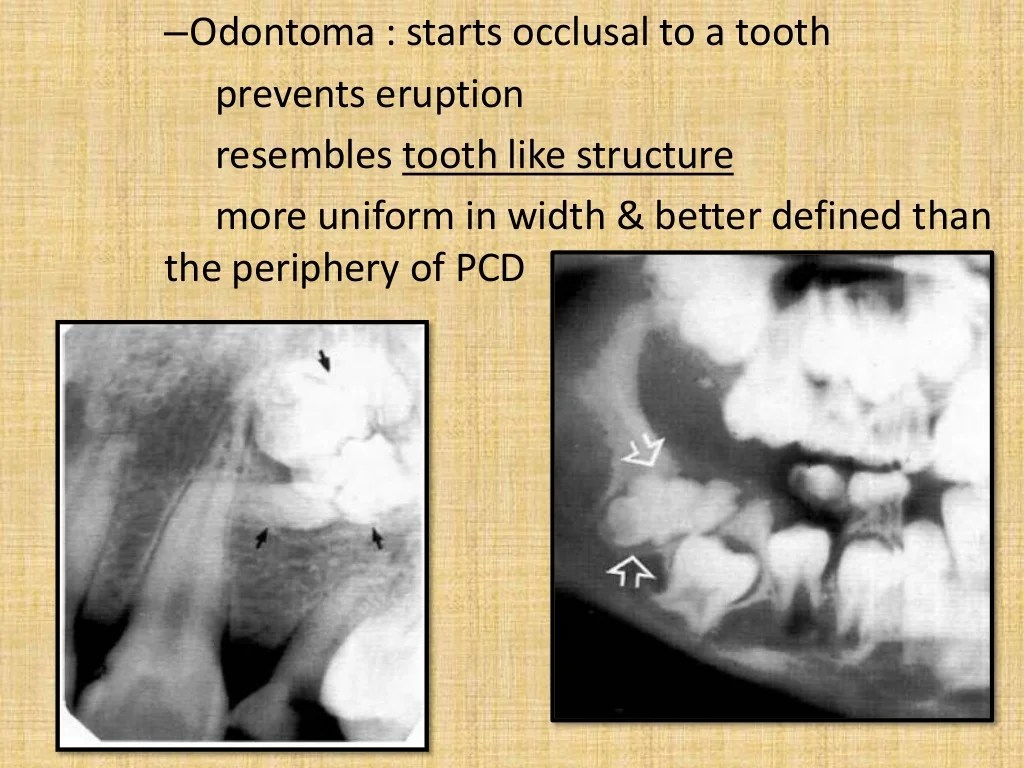
Examples of Radiopaque Lesions
Some common examples of radiopaque lesions found in the mandible include:
- Dental caries:Cavities or tooth decay can appear as radiopaque lesions on X-rays due to the presence of calcified bacteria and debris.
- Osteosclerosis:This condition involves the abnormal hardening of bone, which can result in increased radiopacity on X-rays.
- Paget’s disease of bone:A chronic bone disorder that leads to excessive bone remodeling and can cause radiopaque lesions in the mandible.
- Calcified odontogenic cysts:These cysts are lined with calcified material and can appear as radiopaque lesions on X-rays.
Causes of Radiopaque Lesions in the Mandible: Radiopaque Lesions Of The Mandible
Radiopaque lesions in the mandible can arise from various etiologies. Common causes include dental caries, pulp stones, and calcified dental granulomas. Trauma and infection can also play a role in their formation.
Dental Caries
- Dental caries is a major cause of radiopaque lesions in the mandible.
- As bacteria accumulate on the tooth surface and produce acids, they demineralize the enamel and dentin, creating a carious lesion.
- Over time, the lesion can extend into the pulp chamber, leading to pulpitis and the formation of a periapical abscess.
- The abscess can become calcified, resulting in a radiopaque lesion.
Pulp Stones
- Pulp stones are calcified masses that form within the pulp chamber.
- They are usually asymptomatic but can cause pain if they irritate the pulp tissue.
- Pulp stones appear as small, round, or oval radiopaque lesions on dental radiographs.
Calcified Dental Granulomas
- Calcified dental granulomas are chronic inflammatory lesions that form around the apex of a tooth root.
- They are caused by bacterial infection of the pulp and can appear as well-defined, round or oval radiopaque lesions.
- The calcification process can occur over time, resulting in a more radiopaque appearance.
Trauma
- Trauma to the mandible can lead to the formation of radiopaque lesions.
- Fractures and dislocations can cause bone fragments to become displaced and appear as radiopaque lesions.
- In some cases, trauma can also induce the formation of calcified hematomas, which can appear as radiopaque lesions.
Infection
- Infections in the mandible can also lead to the formation of radiopaque lesions.
- Osteomyelitis, a bacterial infection of the bone, can cause the formation of new bone, which can appear as a radiopaque lesion.
- Fungal infections, such as actinomycosis, can also cause the formation of radiopaque lesions in the mandible.
Clinical Presentation and Diagnosis
Clinical manifestations of radiopaque lesions in the mandible can vary depending on the underlying cause and the extent of the lesion. Common clinical signs and symptoms include:
- Swelling or enlargement of the mandible
- Pain or tenderness
- Asymmetry of the face
- Loose or mobile teeth
- Difficulty chewing or speaking
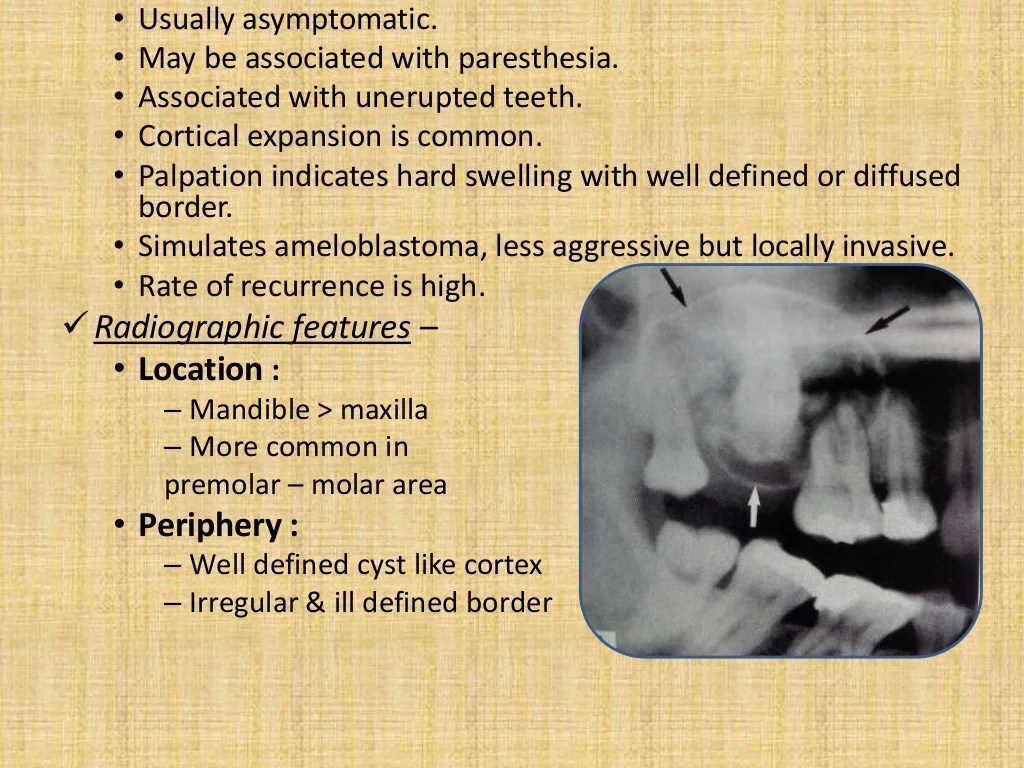
Radiographic imaging, particularly panoramic and cone-beam computed tomography (CBCT) scans, plays a crucial role in the diagnosis of radiopaque lesions of the mandible. These imaging modalities provide detailed views of the mandible, allowing clinicians to assess the size, shape, and location of the lesion.
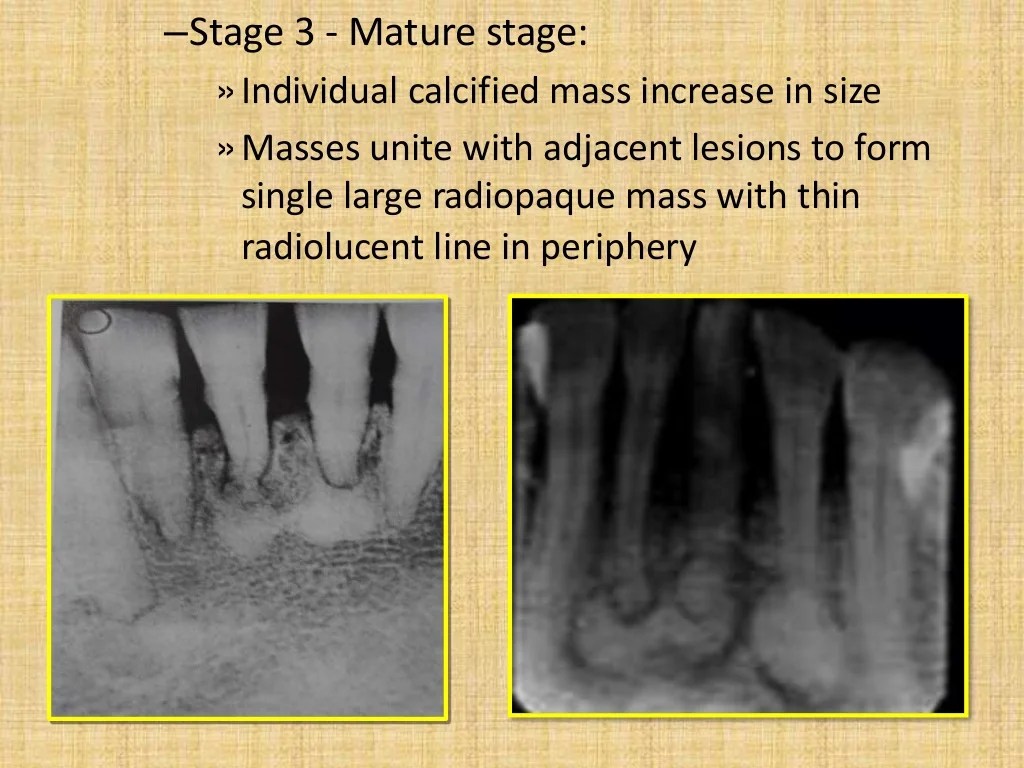
The radiographic appearance of the lesion can help differentiate between various types of lesions:
Interpretation of Radiographic Findings, Radiopaque lesions of the mandible
Radiopaque lesions on panoramic or CBCT scans may appear as:
- Well-defined or ill-defined borders
- Homogeneous or heterogeneous density
- Presence or absence of internal structures
- Involvement of surrounding bone
By carefully interpreting these radiographic findings, clinicians can narrow down the differential diagnosis and determine the most likely underlying cause of the radiopaque lesion.
Differential Diagnosis
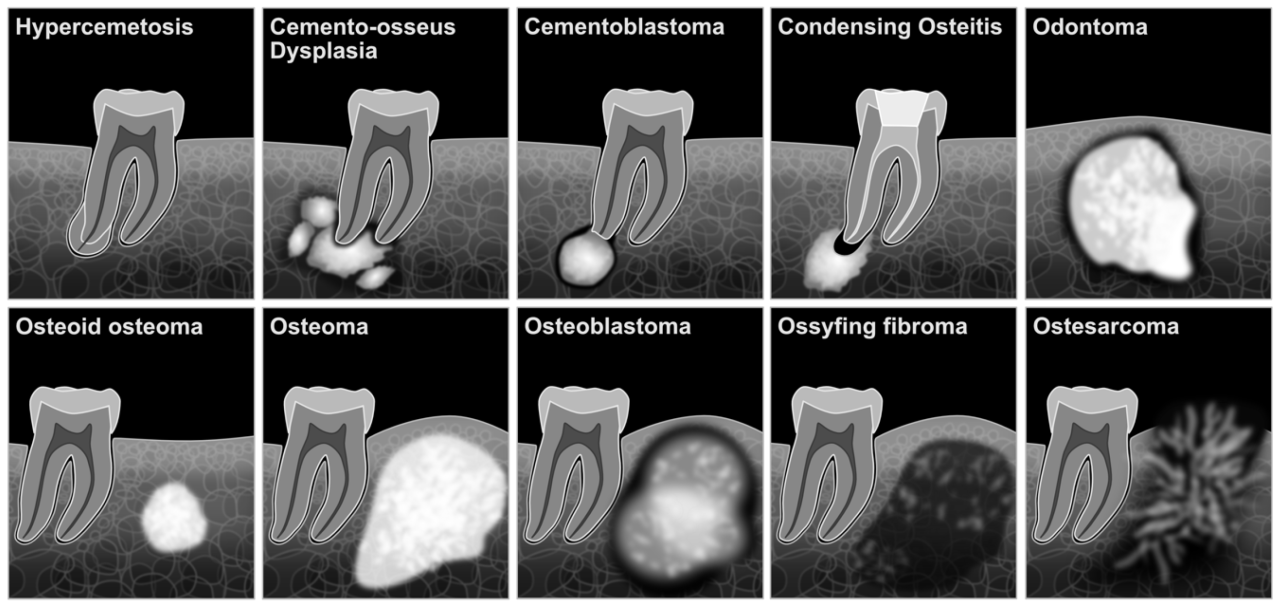
Differential diagnosis is crucial for accurate treatment planning in cases of radiopaque lesions in the mandible. Distinguishing between lesions with similar radiographic appearances helps clinicians narrow down the diagnostic possibilities and determine the most appropriate course of action.
Comparative Table of Radiopaque Lesions
The following table provides a comparison of common radiopaque lesions of the mandible, highlighting their characteristics, location, and associated clinical findings:
| Lesion | Characteristics | Location | Clinical Findings |
|---|---|---|---|
| Osteoblastoma | – Well-defined, expansile lesion with central radiolucency and peripheral sclerosis
|
– Posterior mandible, near the angle | – Pain, swelling, and tooth displacement |
| Cementoblastoma | – Dense, radiopaque lesion attached to the root of a tooth
|
– Root of a mandibular molar or premolar | – Asymptomatic or mild pain |
| Fibro-osseous Lesion | – Mixed radiopaque and radiolucent areas
|
– Posterior mandible, near the angle | – Pain, swelling, and tooth displacement |
| Osteosarcoma | – Irregular, infiltrative lesion with poorly defined borders
|
– Any part of the mandible | – Pain, swelling, and tooth mobility |
Treatment Options
The treatment of radiopaque lesions of the mandible depends on several factors, including the size, location, and underlying cause of the lesion. Treatment options range from conservative measures to surgical intervention.
The following table Artikels the treatment options for radiopaque lesions of the mandible:
| Treatment Modality | Indications | Potential Outcomes |
|---|---|---|
| Observation | Small, asymptomatic lesions | Spontaneous resolution or stabilization of the lesion |
| Medical Management | Inflammatory or infectious lesions | Resolution or reduction of the lesion |
| Surgical Resection | Large, symptomatic lesions or lesions with malignant potential | Complete removal of the lesion |
Prognosis and Prevention
The prognosis of radiopaque lesions in the mandible depends on the underlying cause and the effectiveness of treatment. Early diagnosis and appropriate management are crucial for a favorable outcome.
Preventive measures can help reduce the risk of developing these lesions. Regular dental checkups and proper oral hygiene are essential for maintaining good oral health and detecting any potential issues early on.
Prognosis
The prognosis of radiopaque lesions of the mandible varies based on the underlying cause. Benign lesions, such as osteomas or exostoses, typically have a good prognosis with minimal impact on oral function. Malignant lesions, such as osteosarcomas or metastatic tumors, require aggressive treatment and may have a poorer prognosis.
Prevention
Preventive measures can help reduce the risk of developing radiopaque lesions in the mandible. These include:
- Regular dental checkups to detect and address any potential issues early on
- Maintaining good oral hygiene by brushing and flossing regularly to prevent dental caries and periodontal disease
- Avoiding tobacco use and excessive alcohol consumption, as these habits can increase the risk of oral cancer
- Eating a healthy diet rich in fruits, vegetables, and whole grains to support overall health and well-being
- Protecting the mouth from trauma by wearing a mouthguard during contact sports or other high-risk activities
FAQ
What are the most common causes of radiopaque lesions in the mandible?
Dental caries, pulp stones, and calcified dental granulomas are among the most frequently encountered causes of radiopaque lesions in the mandible.
How are radiopaque lesions of the mandible diagnosed?
Radiographic imaging, particularly panoramic and periapical radiographs, plays a crucial role in the diagnosis of radiopaque lesions of the mandible.
What are the treatment options for radiopaque lesions of the mandible?
Treatment options for radiopaque lesions of the mandible vary depending on the underlying cause and the extent of the lesion. Conservative approaches, such as observation and monitoring, may be appropriate for small, asymptomatic lesions, while surgical intervention may be necessary for larger or more aggressive lesions.